Table of contents
Introduction
If you have PCOS, you may have heard that it can increase your risk of miscarriage — a thought that can be worrying when you’re trying to conceive. The truth is more nuanced: most women with PCOS go on to have healthy pregnancies and babies, but certain PCOS-related factors do make early loss more likely.
In this article, we’ll explain why miscarriage is more common in PCOS, what factors play a role, and most importantly, what you can do to support a healthy pregnancy.
👉 Want to understand PCOS and fertility more broadly? Read our guide: How to Get Pregnant with PCOS.
Does PCOS increase miscarriage risk?
The short answer is yes — studies suggest that miscarriage rates in women with PCOS can be 2–3 times higher than in women without PCOS. But it’s important to note:
-
PCOS ≠ infertility. Most women with PCOS eventually conceive successfully.
-
Miscarriage is not always preventable. Many cases are due to chromosomal abnormalities in the embryo.
-
The risk is linked to hormonal imbalances, insulin resistance, inflammation, and progesterone deficiency — factors you can often address proactively.

Why miscarriage risk is higher in PCOS
1. Irregular cycles and fewer ovulations
With PCOS, cycles can stretch to 40, 60, or even 90+ days. Fewer ovulations = fewer chances per year to conceive. Irregular cycles may also affect egg quality and uterine preparation.
2. Egg quality issues
Egg maturation can be disrupted in PCOS. Higher androgen levels and prolonged follicular phases can result in eggs of lower quality, which increases the risk of failed implantation or early miscarriage.
3. Insulin resistance
Around 70% of women with PCOS have insulin resistance. High insulin disrupts ovulation hormones, increases testosterone, and worsens egg quality. It also reduces SHBG (sex hormone-binding globulin), leaving more free testosterone in the bloodstream.
✨ Supporting insulin sensitivity is one of the most effective ways to reduce miscarriage risk.
-
Eat a low-GI, balanced diet
-
Move daily (even a short walk after meals)
-
Support blood sugar with supplements like Sugar Balance or the Balance Bundle.
4. Progesterone deficiency
Progesterone prepares and maintains the uterine lining. Women with PCOS often produce too little progesterone after ovulation, making it harder for the embryo to implant and increasing the risk of very early miscarriage.
Tip: Ask your doctor for a progesterone test 7 days post-ovulation or at the start of pregnancy. Levels should be at least 15–20 ng/ml. If they are lower, supplementation may help.
5. Inflammation
Low-grade chronic inflammation is common in PCOS. It can disrupt the follicular environment, worsen insulin resistance, and reduce egg quality.
-
Anti-inflammatory diet (limit ultra-processed foods, sugar, alcohol)
-
Omega-3s (from diet or supplements)
-
Gut health support (fibre, probiotics, glutamine if needed)
6. Thyroid issues
Women with PCOS are three times more likely to develop hypothyroidism or Hashimoto’s thyroiditis, both of which are linked to miscarriage.
-
Request a full thyroid panel (TSH, T3, T4, antibodies, iodine status).
-
Target TSH < 2.5 mUI/l when trying to conceive or in early pregnancy.
How to lower miscarriage rsisk with PCOS
Improve egg quality (start 3+ months before conception)
-
Eat a Mediterranean-style diet (protein, healthy fats, complex carbs).
-
Sleep 7–9 hours per night.
-
Reduce stress (yoga, journaling, mindfulness).
-
Supplement smartly:
-
Inositol: supports insulin sensitivity + egg maturation.
-
Quatrefolic® (active folate, B9): reduces miscarriage risk and neural tube defects.
-
Vitamin D, iodine, zinc, B12: key micronutrients often deficient in PCOS.
-
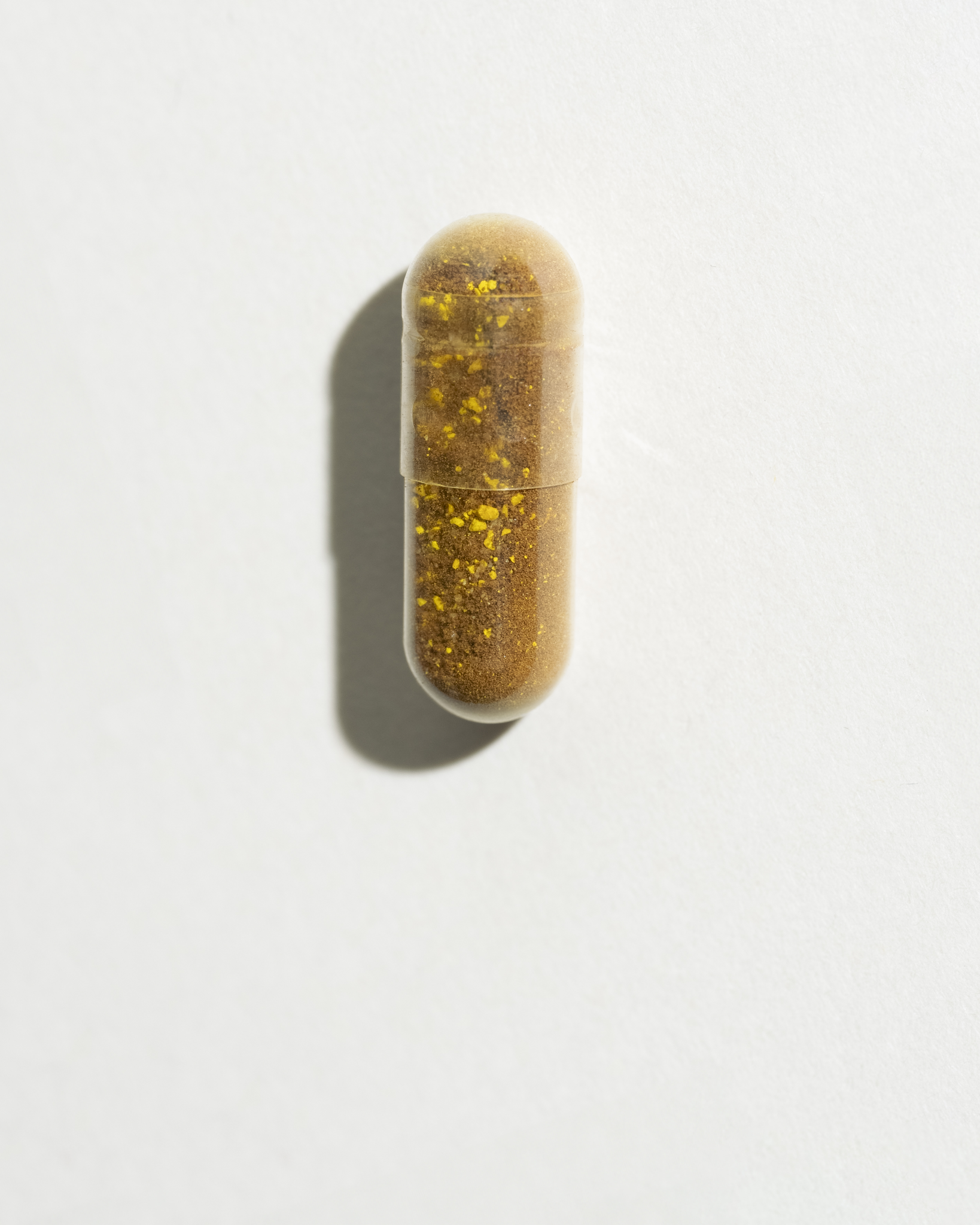
👉 Ovastart combines myo-inositol, Quatrefolic®, zinc, and B6 to support egg quality, ovulation, and cycle balance.
Test and Support Your Hormones
-
Progesterone: check luteal phase levels, supplement if low.
-
Thyroid: test comprehensively, treat if hypothyroidism is detected.
-
Insulin resistance: monitor HbA1c, fasting insulin, and glucose tolerance tests.
Involve Your Partner
PCOS isn’t the only factor in fertility. Around 30% of infertility cases are male-related. Encourage your partner to get tested and adopt fertility-friendly lifestyle habits too.
Final Thoughts
While PCOS does increase miscarriage risk, it doesn’t mean you can’t have a healthy pregnancy. By addressing insulin resistance, supporting egg quality, monitoring progesterone and thyroid function, and reducing inflammation, you can significantly lower your risk.
If you’ve experienced a miscarriage, remember: you are not to blame. Many factors are beyond your control, and support is available. 💜
👉 Ready to take action? Try our 2-minute product quiz for personalised supplement advice to support your fertility journey.
SOVA was created by two sisters with PCOS who wanted products that truly worked. Our formulas are developed in-house with women’s health and micronutrition experts, using ingredients backed by clinical studies and compliant with European regulations.
- Built by women with PCOS, we know the reality of the symptoms.
- Clinically studied, high-quality ingredients, including patented forms like Quatrefolic® and an optimal Myo-/D-Chiro Inositol ratio.
- Holistic support for hormonal balance, metabolic health, inflammation, mood and cycle regulation.
- Transparent, science-led formulas with no unnecessary additives.