Table of contents
To help your body regain hormonal balance, you've probably heard that detoxifying your liver can be beneficial. However, you may still wonder what the connection is between your hormones and your liver! In this article, we’ll explain how PCOS affects liver function and how to take care of your liver when you have PCOS — and when supplements like Ovastart or the Balance Bundle could play a role in supporting your hormonal reset.
The Liver: definition and functions
A digestive organ

The liver is part of your digestive system and plays numerous roles. Located under the diaphragm and partially protected by the ribs on the right side, it’s filled with blood and weighs about 2.4 kg.
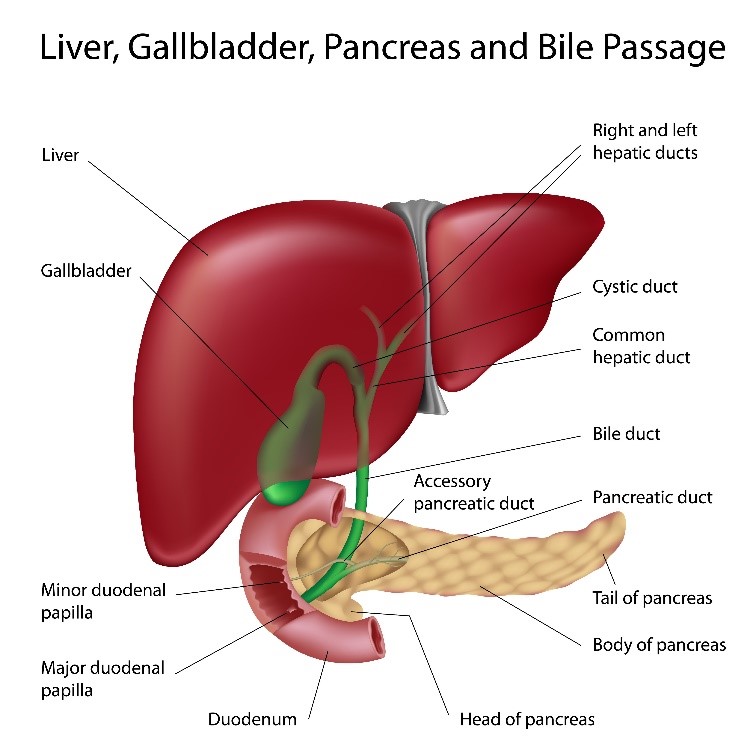
In addition to being an organ, the liver is also a gland because it produces bile—its only digestive function. Bile is a fluid that emulsifies fats so they can be properly digested.
Beyond this digestive role, the liver’s main function is to process nutrients.
The various functions of the liver
The liver performs three other key functions that are especially important to monitor if you have PCOS or other hormonal imbalances.
Metabolic and regulatory functions
Think of the liver as a mini factory, transforming and storing the nutrients you consume after each meal.
For example, the liver is responsible for storing glucose as glycogen to maintain normal blood sugar levels. After meals, carbohydrates are converted into glycogen and stored in the liver.
When blood sugar levels drop, the liver breaks down these large glycogen molecules to release sugar into the bloodstream, stabilising blood sugar levels and providing energy.
Protein synthesis
The liver produces essential proteins for the body’s functioning, such as albumin, which transports hormones, calcium, and fatty acids in the blood.
It also produces:
-
Globins, which store and transport oxygen
-
Coagulation factors to stop bleeding and aid in healing
-
Iron metabolism proteins (ferritin and transferrin)
-
Lipoproteins that transport lipids (fats), including cholesterol, in the blood
Detoxification
This is the liver function you’ve probably heard the most about! The liver breaks down toxic substances, such as alcohol, medications, and ammonia (a byproduct of digestion that is toxic to the brain).
In the next section, we’ll focus on detoxification so you can understand how it works and why supporting this process is important if you have PCOS or hormonal imbalances.
Liver detoxification
As mentioned earlier, the liver transforms, regulates, synthesises, and breaks down nutrients. These functions all contribute to liver detoxification, which occurs in three phases.
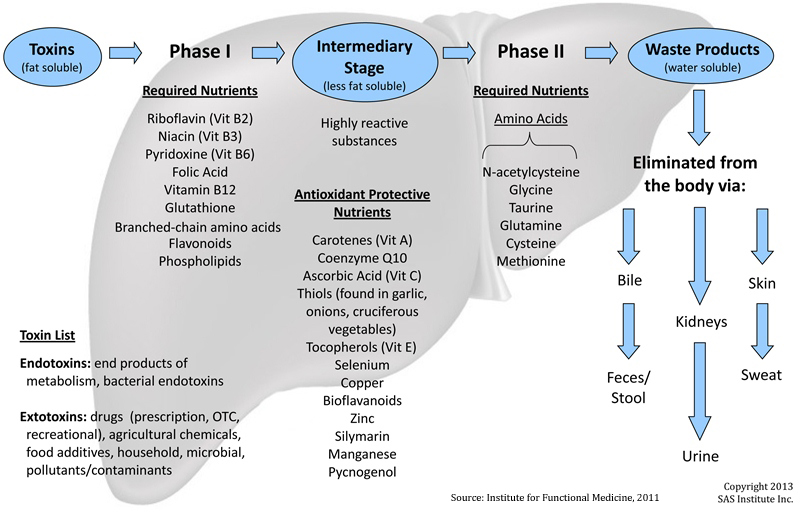
Phase 1
Phase 1 is the activation phase, the first line of defence against toxins. The liver begins breaking down toxic substances into simpler compounds using enzymes called cytochrome P450. These enzymes make toxins more reactive and water-soluble.
However, this phase doesn’t eliminate all toxins, and some byproducts can become even more toxic. That’s why it’s important to support phase 2 of liver detoxification alongside phase 1.
Phase 2
Phase 2 is known as the conjugation phase. In this stage, toxins are bound to other substances, such as glutathione (an antioxidant) or amino acids, to make them less toxic and more water-soluble. This process requires a lot of energy and nutrients.
Once toxins are conjugated, the body can eliminate them through urine and stool.
Phase 3
The final phase is elimination, where toxins are excreted from the liver. Toxins leave the liver via bile, which flows into the intestines and is excreted through stool, or they are filtered through the kidneys and excreted in urine.
To support the entire liver detoxification process, it’s essential to ensure regular bowel movements to help eliminate waste effectively.
Now that you understand the detoxification process, let's look at how PCOS, a hormonal imbalance, can disrupt this system.
How does PCOS disrupt liver detoxification?
PCOS is characterised by insulin resistance, excess androgen hormones, and chronic inflammation, often resulting in irregular cycles, acne, hirsutism (excess hair growth), hair loss, and chronic fatigue.
Let’s explore how these three key features of PCOS impact the liver.
Insulin Resistance
In recent years, an increasing number of women with PCOS have been diagnosed with non-alcoholic fatty liver disease (NAFLD). (1) NAFLD is marked by fat (triglyceride) accumulation in the liver, which can lead to inflammation and toxicity, potentially causing liver fibrosis (scarring). Fortunately, lifestyle changes and managing associated conditions like PCOS can reverse this trend and relieve the liver of this fat overload.
We mention this condition to highlight the connection between PCOS and liver detoxification.
Indeed, insulin resistance , one of the main symptoms of PCOS, increases the risk of developing fatty liver disease. (2) High levels of insulin in the blood disrupt the liver’s detoxification phases, particularly phases 1 and 2, which involve making fats (toxins) water-soluble for excretion. When this process is compromised, the liver accumulates fat and toxins, leading to chronic inflammation in the liver. (3)
Supplements like Sugar Balance were created to support healthy blood sugar levels and metabolic balance — a key step in reducing the burden on your liver.

Hyperandrogenism
Excess androgen hormones (hyperandrogenism) also affect liver function and play a role in fatty liver disease development in women with PCOS.
A link has been established between excess androgen hormones, hyperinsulinemia, and obesity, but it is unclear whether hyperandrogenism or insulin resistance disrupts liver function. (4) Some studies suggest that hyperinsulinaemia can lead to hyperandrogenism, while others suggest that hyperandrogenism contributes to NAFLD development even in women with PCOS who have a normal BMI and no insulin resistance. (4)
In simple terms, hyperandrogenism is believed to cause metabolic disturbances, including those of the liver, regardless of body fat percentage or weight in women with PCOS. (5)
Want to know more? Check out our article dedicated to Excessive Hair Growth and PCOS.
Chronic inflammation
PCOS is associated with low-grade chronic inflammation, which has effects similar to metabolic syndrome. (6)
According to INSERM, metabolic syndrome is characterized by a waist circumference over 80 cm for women, hyperglycaemia, elevated triglycerides, low HDL cholesterol, and/or high blood pressure. Although this syndrome remains silent for a long time, it increases the risk of liver disease, cardiovascular diseases, and type 2 diabetes.
In the case of PCOS, low-grade chronic inflammation is sustained by insulin resistance, hyperandrogenism, and an excess of fat cells called adipocytes. (6) These three factors increase fat accumulation in the liver, promote inflammation, reduce liver detoxification capacities, and disrupt nutrient metabolism.
Unfortunately, the main symptoms of PCOS—insulin resistance, hyperandrogenism, and chronic inflammation—can disrupt liver function, exacerbating and perpetuating PCOS symptoms.
So, how can you support your liver if you have PCOS?
Targeting inflammation holistically — through lifestyle, nutrition, and the right supplements — can help your liver function more smoothly. Our Balance Bundle combines our two core formulas to support hormonal balance and healthy blood sugar levels in one simple routine.
How to ensure proper liver detoxification when you have PCOS
To ensure effective liver detoxification and reduce the risk of developing fatty liver, it’s essential to support each phase of liver detoxification. The best approach is to start with phase 3 and work backwards to phase 1, ensuring that toxins are properly eliminated.
Phase 3: Improve bowel movements
In this phase, the goal is to stimulate waste elimination through urine and stools. Here are some tips to improve your digestive transit and support toxin removal:
-
Drink 1 to 2 litres of water throughout the day to help flush out toxins via urine and regulate your bowel movements.
-
Eat fibre-rich foods, which act as an “intestinal broom” to help prevent constipation. You can find fibre in fruits, vegetables, grains, and legumes. For more information on PCOS-friendly nutrition, check out our article.
-
Add psyllium to your diet. This plant, which swells when in contact with water (similar to chia seeds), eases bowel movements and helps stimulate intestinal activity. For example, add 1 to 2 teaspoons of psyllium daily to yogurt, applesauce, or porridge for three weeks.
-
Walk daily to promote bowel movements.
-
See an osteopath or try belly massaging to relieve tension and regulate your bowels. This is particularly useful if you tend to feel stress in your abdomen.
Phase 2: supply amino acids and antioxidants
This phase requires a lot of amino acids and antioxidants for the liver to detoxify properly.
Here are some ways to support this second phase of detox:
-
Eat foods rich in sulfur-containing amino acids, such as eggs, garlic, onions, and broccoli, which help the liver bind toxins.
-
Ensure adequate protein intake to provide the amino acids needed for phase 2 of detoxification. To increase your daily protein intake, try a savoury breakfast with eggs. If you’re vegan, opt for complete proteins like soy, quinoa, and combinations of legumes and grains to provide all the amino acids your body needs.
-
If you’re prone to stress, consider a magnesium supplement to support this detox phase. Magnesium stores deplete quickly when you’re stressed or anxious.
-
Supplementing with L-glutamine is also beneficial if you suffer from digestive issues like bloating, pain, constipation, or diarrhoea. This amino acid supports detoxification, reduces intestinal permeability, and soothes digestive inflammation.
Phase 1: Boost Your Vitamin Intake
Phase 1 is the most vitamin-dependent, particularly when it comes to B vitamins. Deficiencies in vitamins B2, B3, B6, B9, or B12 can impair the first phase of toxin detoxification.
Ovastart includes active folate (Quatrefolic®), vitamin B6, and zinc — key nutrients to support this phase of detoxification and overall hormonal balance.
Here are some tips to support the first detox phase:
-
If you’re taking the contraceptive pill, consider a vitamin supplement, particularly B vitamins, to support your liver. The pill can deplete certain vitamins, slowing down liver function.
-
If you’re vegan, it’s crucial to supplement with vitamin B12, which isn’t available in plant-based foods. The Vegan Society recommends either eating fortified foods two or three times a day to get at least 3 micrograms of B12 a day, or taking cyanocobalamin at 10 micrograms daily, or 2,000 micrograms weekly.
-
Eat nutrient-rich foods that support liver enzymes, such as cruciferous vegetables (cabbage, broccoli), citrus fruits, avocados, and berries.
-
Add spices and herbs like turmeric, ginger, rosemary, and dandelion to your diet. These are rich in flavonoids, which are beneficial for phase 1 detoxification. You can also enjoy ginger, rosemary, and dandelion in teas.
-
Minimise exposure to environmental toxins and hepatotoxic (liver-toxic) substances, such as alcohol and endocrine disruptors found in cosmetics, hygiene products, disposable menstrual products, plastic, and perfumes. Reducing your toxin exposure means your liver has less work to do.
Addressing the Root Causes to Relieve Symptoms
Most of these tips aim to reduce the liver’s workload, but they won’t optimise its function unless the underlying causes of PCOS are addressed. Tackling insulin resistance, hyperandrogenism, and chronic inflammation is key to relieving the pressure on your liver and helping your body find balance again.
That’s why we created Ovastart, a blend of myo‑inositol, D‑chiro‑inositol, zinc, and active folate to support hormonal and menstrual health, and Sugar Balance, designed to promote healthy blood sugar levels and metabolic balance. For those who want the benefits of both in one simple routine, the Balance Bundle combines these formulas to address the key drivers behind PCOS-related liver strain.
We encourage you to reach out to health and wellness professionals for guidance, and to view supplements as part of a broader, holistic approach to PCOS management — one that supports your liver, your hormones, and your overall well-being.
✨ Not sure which one is right for you? Take our free quiz here to get a personalised recommendation.
Scientific references
SOVA was created by two sisters with PCOS who wanted products that truly worked. Our formulas are developed in-house with women’s health and micronutrition experts, using ingredients backed by clinical studies and compliant with European regulations.
- Built by women with PCOS, we know the reality of the symptoms.
- Clinically studied, high-quality ingredients, including patented forms like Quatrefolic® and an optimal Myo-/D-Chiro Inositol ratio.
- Holistic support for hormonal balance, metabolic health, inflammation, mood and cycle regulation.
- Transparent, science-led formulas with no unnecessary additives.