Table of contents
Have you ever heard of insulin resistance? If so, you might be among the 75% of women with PCOS who have also been diagnosed with this resistance.
But what exactly is insulin resistance, and how does it impact PCOS? In this article, we’ll break it down and share how you can manage it to better balance your hormones.
👉 Not sure where to start? Take our free PCOS product quiz to get a personalised routine that supports hormonal balance and blood sugar regulation.
What is Insulin Resistance?
To fully understand your PCOS, you first need to grasp the different mechanisms and processes involved. Insulin resistance is now recognised as one of the main drivers of Polycystic Ovary Syndrome. That’s how important this topic is to us!
Insulin resistance… OK… but what exactly is it?
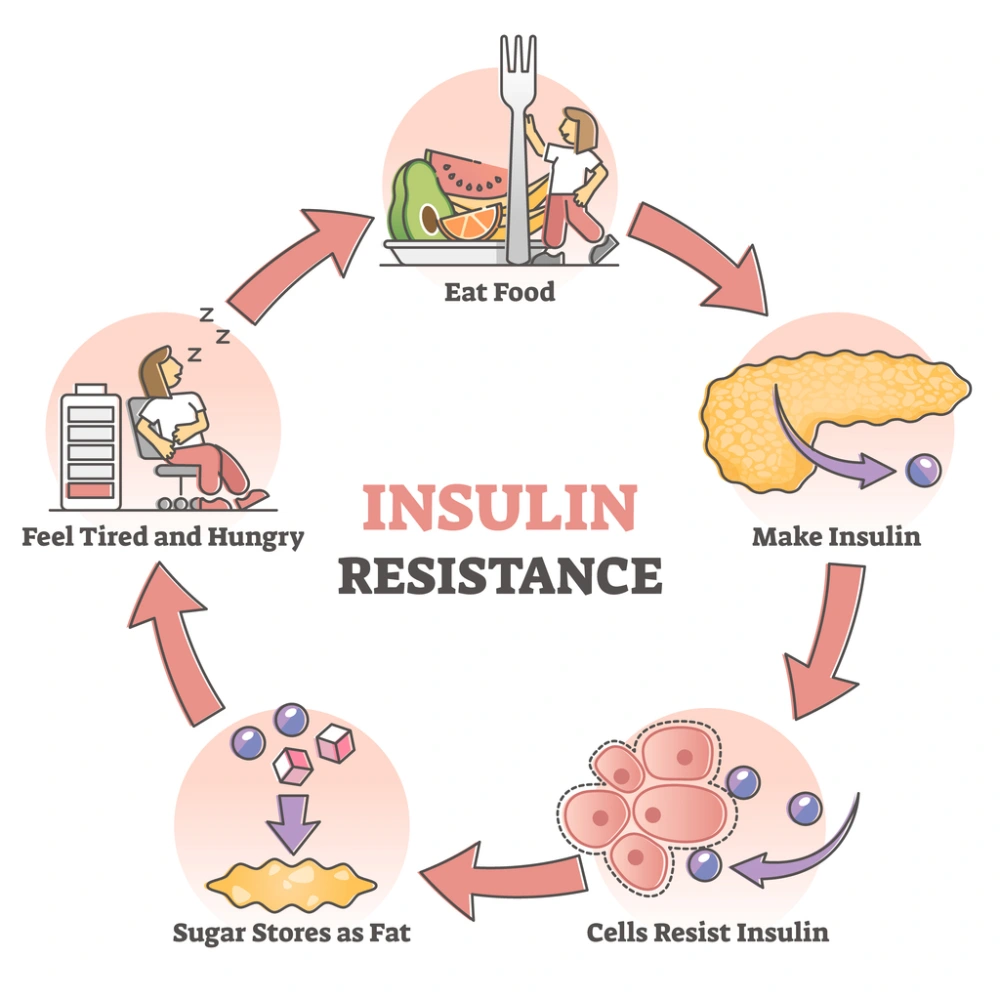
It’s an inflammatory condition in which the body gradually becomes less sensitive to glucose — in other words, to “sugars”.
To deal with the waves of sugar from our diet, the body produces a hormone called insulin. This hormone is secreted by the pancreas as soon as it detects an influx of glucose in the blood (whether that’s after a meal or even due to stress). For example, when we eat a plate of pasta, some bread with a few squares of chocolate (we know you… most of us are the same!), or even a simple salad, the sugar from these foods is digested and absorbed. Once it reaches the pancreas (specifically the beta cells), it triggers the release of tiny vesicles containing insulin.
Once released, insulin can get on with its main job: lowering blood sugar levels (glycaemia) by allowing glucose to enter our cells — in the liver, muscles, and fat tissue. Think of it as the key that unlocks the door to your cells for glucose.
How does insulin actually get glucose inside the cell? It binds to specific receptors (the locks for the famous key!) located on the surface of target cells. This key-and-lock interaction sends a signal to the cell, which then opens up and lets the glucose in.
But why do our cells need glucose in the first place? Simply because carbohydrates — the “sugars” in our diet — are their main source of fuel. Without glucose, cells can’t produce energy or function properly. We really do need these sugars!
How does insulin resistance develop?
For a variety of reasons (often combined), prolonged high blood sugar — and therefore high insulin — makes cells more resistant to insulin’s message. If the message isn’t received… the door stays shut, and glucose remains outside the cell.
As more sugar builds up in the blood, the pancreas works harder, producing more insulin in an attempt to get glucose inside the cells. If this cycle isn’t interrupted, the pancreas eventually becomes exhausted, leading to pre-diabetes or type 2 diabetes.
What's the link between insulin resistance and PCOS?
As mentioned earlier, insulin resistance leads to hyperinsulinaemia (high insulin levels in the blood). Excess insulin directly disrupts the hormonal system:
-
It stimulates testosterone production (through LH), creating an imbalance with FSH. This means male hormones are less likely to convert into female hormones, leading to hyperandrogenism (excess androgens).
-
It lowers SHBG (a protein that binds testosterone), leaving more “free” testosterone active in the blood — the form responsible for symptoms such as acne, hirsutism or hair loss.
This is why taking care of insulin balance is particularly important with PCOS.
⚠️ Remember: PCOS is multifactorial. Insulin resistance is one part of the picture, but inflammation or other factors may also be at play.
To help you, we have written articles on inflammatory-type PCOS and adrenal PCOS, feel free to check them out!
What are the symptoms of insulin resistance and how to diagnose it?
First of all, it is good to know that insulin resistance can sometimes go unnoticed for several years. Why is that? The pancreas compensates by producing more insulin, keeping blood sugar levels within a “normal” range.
Some women may therefore not experience any of the symptoms mentioned below. It is very important to talk to your doctor, and / or your gynaecologist and / or your endocrinologist if you have any doubts.
Signs that your body is resisting insulin:
In the meantime, here is a (non-exhaustive) list of the most common signs:
- An increase in waist circumference with excess abdominal fat (that little belly pouch that has grown and that we can’t seem to be able to get rid of... Even for the slimmest among us!).
- Extra pounds slowly piling up (remember, insulin is also responsible for fat storage!) and more difficult weight loss.
- Fatigue (in case of hyperinsulinemia, energy becomes difficult to mobilise, leading to chronic fatigue), a sign very often found with PCOS.
- Sugar cravings, sometimes incessant hunger throughout the day.
- Chronic migraines.
- Increasingly poor memory and concentration (not knowing where we put our keys doesn’t count... It happens to all of us).
If any of these sound familiar, it’s worth speaking to your doctor. Beyond glucose and insulin levels, useful markers include:
- HbA1c: It reflects your blood sugar level over a relatively long period (2 to 3 months). If you are not diabetic, this should ideally be below 5.4%, according to several doctors.
- HOMA: It measures your level of insulin resistance. This test should be done fasting (for 12 hours). According to scientific literature, the index should ideally be below 2.4, or even a bit less according to some researchers...
- QUICKI: It measures your insulin sensitivity. Unlike the HOMA test, the higher this index, the better! Ideally, it should be above 0.34.
- SHBG: Here we find our testosterone carrier which is very interesting to measure in the context of potential insulin resistance. The lower this marker, the more likely you are to be diagnosed with insulin resistance.
- Other useful markers: Vitamin D, Vitamin A / RBG, Chromium, Erythrocyte Magnesium, Iodine (urine iodine analysis)

Why does the body resist insulin?
Insulin resistance can be caused by, or worsened for, many reasons. Genetics is one of them, but it does not mean that we cannot rebalance our insulin.
If we set aside certain periods of life, such as pregnancy, puberty, or ageing, which can affect our sugar balance, we find the following potential causes:
- First of all, hyperinsulinemia itself, that is, too much insulin in our blood (caused by an ever-increasing production from our pancreas trying to cope with too much sugar… We're getting there!).
- Excess weight and/or simply an inappropriate or overly rich diet (but not necessarily rich in good nutrients!).
- Chronic stress will increase our blood sugar and thus exacerbate insulin resistance through the production of cortisol (our dear stress hormone!). Cortisol makes the receptors on our cells, where insulin is supposed to bind, insensitive.
- Sedentary lifestyles: movement maintains our muscle fibres which will, in turn, demand insulin.
- Elements interfering with the insulin message: a cell with an outer membrane that is not fluid enough to let the message through (lack of Omega-3 fatty acids, for example), insulin receptors that do not activate due to some nutrient deficiency (Magnesium, Zinc, Chromium).
- Mitochondrial dysfunction (we will return to this magnificent element, the mitochondrion, present in large quantities in our cells, in a future article!). These entities are responsible for producing our energy by converting glucose that enters our cells (and so, if there are not many functional mitochondria… There is a lot of free glucose!).
- Smoking, which increases our insulin.
- Hypothyroidism, i.e., an underactive thyroid: to learn more, visit PCOS and Hypothyroidism, What’s the Link?
- Digestive disorders (Yes… They are everywhere!).
- And other possible cause-effect links…
How to Overcome Insulin Resistance?
The aim isn’t to cut out sugar completely (our bodies need it) but to keep blood sugar stable. Think of gentle hills rather than sharp peaks.
Your mission, should you choose to accept it? Try the recommendations that resonate with you the most amongst the following and do not hesitate, to go further, to seek support from a naturopath or a nutritionist specializing in PCOS.
Our tips to restore stable blood sugar levels:
From a dietary perspective, here is what you can already implement (of course, personalise it with support):
Tip #1: Establish a sort of food chronobiology
- A breakfast rich in proteins and good fats: avoid sugar-rich foods in the morning (breakfast cereals, fruit juices including homemade, white bread baguette…).
- If time allows, you can delay your breakfast a bit to engage in gentle activity in the morning (walking, stretching, gentle yoga…).
- A balanced lunch with carbohydrates: this is the right meal for you to introduce cereals (pasta, rice, but also quinoa, bulgur, amaranth, millet…) and starchy foods (sweet potato, potato…), which you can come with animal or vegetable proteins (lentils, chickpeas…), and of course vegetables! You can try consuming fibres (vegetables here) first, then proteins and fats (meat, fish, lentils with your favourite oil…), and finally your carbohydrates (this will slow down glucose absorption).
- A light dinner: a light meal with minimal carbohydrates will help avoid storage during the night (especially if you eat late). Why not eggs or fatty fish with vegetables?
- Avoid desserts in the evening and prefer them, if necessary, after lunch (but you can occasionally have your chocolate while watching a movie in the evening… Don’t forget the little pleasures!).
Tip #2: Smooth out your meals throughout the day!
Wanting to avoid big blood sugar spikes means not skipping meals at random, but also not snacking non-stop. We recommend learning gradually to listen to your hunger (it takes time, but you will get there eventually!).
Tip #3: Favour raw foods!
It is important to favour raw and minimally processed foods (to go back to the basics of a PCOS diet). To help along the way, you can read our article on Diet and PCOS.
Prefer raw vegetables over commercial soups, whole fruits over fruit juices…
And enjoy fruits/vegetables, nuts, good oils (olive ++, walnut, hemp…), legumes, whole grains, fatty fish…

Tip #4: Limit foods containing a lot of added sugars.
It is important to limit foods that contain a lot of added sugars, whether glucose or fructose (cookies, sodas, fruit juices, dried fruits like dates, alcohol, overripe fruits…).
Be careful also with processed frozen foods and canned goods that often contain sugar (yes, even in savoury dishes!)... And with salty foods too (excess salt would promote excessive sugar absorption!).
It is important to apply all these tips while keeping some of your comfort foods (we don’t want to completely eliminate them but rather limit their intake: everything is a matter of balance).
Tip #5: Favour low glycemic index (GI) and low glycemic load (GL) foods.
By creating wholesome dishes as suggested above.
You can also eat cereals and starchy foods by cooking them, then cooling them in the refrigerator (to have them cold or reheated). This helps limit blood sugar spikes when eating them! And of course, avoid overcooking them (favour al dente pasta, for example).
Tip #6: Use your glucose!
By promoting movement (move, go out, practice 10 to 20 minutes a day of physical activity, ideally after meals).
The important thing is regularity: 10 minutes a day of gentle activity will be more beneficial for you than 1 hour of intense cardio done only on the weekend (though that’s already quite good!).
Tip #7: Occupy your nervous system!
Take care of your nervous system… That means managing your stress (sport, breathing, relaxation, meditation, reading, writing… Whatever helps you to chill out!).
Use plants: nigella, berberine, cinnamon, schisandra chinensis, ginger, turmeric, juniper or olive buds…
Again, adapt all that with the healthcare professional of your choosing!
Berberine, for example, will help our body increase its sensitivity to insulin, thereby helping to reduce insulin resistance. It is both hypoglycemic (i.e. lowering blood sugar levels), and an activator of our metabolism, to reset our functions. Be careful, it is contraindicated during pregnancy (also be careful during an ongoing “pregnancy project”!). For the record, berberine is said to have similar effects to Metformin, a medical treatment used against type II diabetes.
Tip #8: Help from micronutrition!
To go the extra-mile, you can get help from micronutrition: inositol, zinc, chromium, omega-3, magnesium, coenzyme Q10, L-theanine… to be adapted to your problem (watch out for contraindications).
Inositol, unlike berberine for example, is interesting when trying to have a baby and during early pregnancy (and so much more!). Naturally present in our body, it has a direct effect on our insulin by improving its action. It is also interesting with PCOS as it improves the quality of our oocytes and allows us to optimise ovulation. Many studies have proven its effectiveness on fertility and the regulation of our hormonal system (let’s take advantage of that!).
At Sova, we have several product ranges. Notably, Ovastart, a combination of molecules supporting hormonal and menstrual health by promoting hormonal regulation and balance.
To learn more about this must-take inositol, you can also read our article on Inositol and PCOS.
You will also find chromium in our product Sugar Balance a complex based on Berberine, NAC, Cinnamon, Gymnema, Green Tea & Chromium. This combination helps maintain glycemic balance, promotes toxin elimination, reduces sugar cravings, and improves post-meal fatigue.
👉 Unsure which one is right for you? Take the Sova product quiz for a personalised recommendation.

Tip #9: See a healthcare professional!
It is also very important to check with your doctor if you have inflammation or thyroid problems. You should also regulate your digestive system with your naturopath if you have issues (by taking care of your liver, which is a crucial passage for all hormones produced by your pancreas, amongst other things!).
Conclusion:
At Sova, we are convinced that knowledge is essential to improve quality of life with PCOS. We hope this article has given you keys to better understand what insulin resistance is and its impact.
But we are not stopping there!
👉 Discover your personalised routine with our PCOS product quiz and explore targeted solutions like Ovastart, Sugar Balance, and Omega-3.
SOVA was created by two sisters with PCOS who wanted products that truly worked. Our formulas are developed in-house with women’s health and micronutrition experts, using ingredients backed by clinical studies and compliant with European regulations.
- Built by women with PCOS, we know the reality of the symptoms.
- Clinically studied, high-quality ingredients, including patented forms like Quatrefolic® and an optimal Myo-/D-Chiro Inositol ratio.
- Holistic support for hormonal balance, metabolic health, inflammation, mood and cycle regulation.
- Transparent, science-led formulas with no unnecessary additives.