Table of contents
Polycystic Ovary Syndrome (PCOS) is a complex disorder that affects both the reproductive system and the metabolism of women. It is a common ailment affecting 8 to 13% of British women of childbearing age.
Beyond the well-known symptoms such as hormonal imbalances, irregular menstrual cycles, acne, or hirsutism, PCOS has profound repercussions on the mental health of those affected.
This article explores the often-overlooked dimension of PCOS—its link to mental wellbeing—while offering strategies and supplement recommendations to help you manage symptoms and find more peace of mind.
A brief overview of PCOS
PCOS is a hormonal imbalance that affects women and can appear as early as puberty or later in life, often after stopping contraception. It is estimated that about 1 in 5 to 10 menstruating women in the UK are affected by this disorder. It is a complex pathology that impacts not only the reproductive system (ovaries) but also the body as a whole (hormone production imbalance from the pituitary gland, adrenal glands, and pancreas).
The most recurring symptoms of PCOS include the absence of menstrual cycles or highly irregular cycles, acne, excessive hair growth, difficulty losing weight, hair loss, infertility, mood disorders, etc. Note that each case of PCOS is unique, and you may not experience all these symptoms at once (Phew!).
👉 Want to learn more about the signs of PCOS? Read our guide on PCOS.
Today, we will focus on the possible mental health consequences of PCOS and share some tips to help you feel better both mentally and physically! 😉

The connection between PCOS and your mental health
PCOS is a complex disorder that can affect you throughout your life. Like many chronic diseases, the burden of symptoms associated with PCOS can have significantly impact your mood, mindset, and ability to manage stress and emotions.
Emotional challenges linked to PCOS
The shock of diagnosis
Often, the diagnosis of PCOS comes as a shock. The lack of understanding of the pathology’s implications, along with sometimes distressing information provided by doctors (infertility, fertility treatments), can negatively impact the patient's mental health (1). Accepting the condition and its symptoms can take time. If you’re diagnosed with PCOS, you may go through phases of disbelief, anger, or even denial. The diagnosis can also come with stigma (“if you have PCOS, it’s because you’re overweight”) and misunderstandings, increasing the emotional burden associated with your symptoms. Uncertainty about long-term implications can also make you anxious about the future, which is entirely normal!
At SOVA, we are here to support you through these sometimes painful processes. 🤗
👉 Not sure what PCOS really means for your future? Start by reading our article on how PCOS is diagnosed for a clear explanation.
Distressing symptoms
Another source of emotional distress related to PCOS involves the physical symptoms themselves. Acne, hirsutism (check out our article Excessive Hair Growth and PCOS: What Are the Solutions?), hair loss (check out our article Alopecia - How to manage Hair Loss with PCOS), or difficulty losing weight (check out our article on How to lose weight with PCOS), can all affect your self-image, leading to insecurities about, and feelings of discomfort in your own body. You may also feel social pressure to minimize these symptoms, which are often deemed aesthetically unacceptable, especially for women.
Irregular menstrual cycles, or their absence altogether, can also cause feelings of inadequacy and the sensation of being “abnormal” or different from other women who don’t have issues with their periods. Not having regular periods can alter your sense of femininity, making you feel like you are not “woman enough” because your reproductive system doesn’t work as it should. This dysfunction can cause anxiety about your fertility and the possibility of conceiving naturally.
Emotional turmoil related to potential infertility
The emotional challenges linked to infertility, which can be associated with PCOS, also have negative impacts on mental health. This includes an increased mental load from the likes of fertility treatments, medical appointments, cycle tracking, and so on. Many women experience feelings of guilt, wondering, "What did I do wrong?" and struggle to comprehend, "Why is this happening to me?” If you’re unable to conceive naturally, medical interventions (fertility treatments, IVF) can disrupt your hormonal balance, leading to mood disorders and even more significant emotional distress (2). Remember that you can get pregnant naturally even with PCOS.
✨ Good news: Many women with PCOS conceive naturally! Learn more in our article How to Get Pregnant with PCOS.
As we’ve seen, PCOS carries significant emotional challenges that can affect your mental health in the long term. Additionally, the physical dysfunctions associated with PCOS can disrupt your internal balance, potentially affecting your psychological wellbeing.
Physiological Consequences of PCOS Influencing Your Mental Health
Hormonal fluctuations and their impact on mental health
Numerous studies have explored the link between PCOS-related hormonal imbalances and the emotional symptoms experienced by patients. One study highlighted an increased risk of developing symptoms such as anxiety and even depression in those with insulin resistance, a common feature of PCOS (3).
Another study revealed a greater tendency towards depression among adolescents with PCOS, linked to elevated male hormones (4). Indeed, elevated male hormones (including testosterone) have been associated with irritability, depression, and more frequent mood swings. Women with PCOS may also experience an imbalance in progesterone production, due to an inverted ratio of LH to FSH hormones (LH being permanently too high). This progesterone deficiency (either in quality or quantity) can affect your mental state since progesterone stabilizes mood when produced in physiological amounts. This deficiency therefore increases the risk of developing a more significant Premenstrual Syndrome (5).
👉 Want to understand this connection better? Read our guide on PCOS and insulin resistance.
The influence of PCOS on brain function
PCOS can also influence the chemical makeup of your brain, altering the production of neurotransmitters—molecules ensuring message transmission from one neuron to another such as dopamine and serotonin— which are essential for mood regulation. A study showed that women with PCOS suffering from depression or anxiety had low serotonin levels(6). Another study suggested that PCOS might be linked to a disruption in communication between the hypothalamus, pituitary gland (both located in the brain), and the adrenal glands, prompting the latter to produce more cortisol, which can alter emotional responses.
Chronic stress and PCOS
When the body is exposed to prolonged stress, the balance of stress hormones is disrupted, and blood cortisol levels (a stress hormone released by small glands located above the kidneys) rise disproportionately, leading to negative effects on both physical and mental health such as high blood pressure, heart problems, weight gain, chronic inflammation, irritability, spasms, etc. (7) Abnormally high cortisol levels have been detected in women with PCOS, linking increased stress markers to physical changes like abdominal weight gain and increased waist circumference. (8) Chronic stress also exacerbates PCOS symptoms by increasing inflammation, insulin resistance, and male hormone production. (9) This worsening of symptoms can further damage self-image, thereby creating some more chronic stress and leading to a vicious circle.
👉 For more information on the link between PCOS and chronic stress, you can read our article about Adrenal PCOS.
The impact of PCOS on mental health stems from both the emotional challenges associated with managing the condition and the hormonal imbalances resulting from the syndrome. Next, we’ll discuss the social costs of living with PCOS and its consequences on mental health.
Social stigma and PCOS
Often, PCOS alters your appearance through weight gain, excessive hair growth, hair loss, or acne. These "imperfections" conflict with societal beauty standards, which are not very tolerant of differences. In social interactions, PCOS is frequently associated with myths and misconceptions like "Just eat better and exercise, and you'll lose weight", "You should get permanent hair removal for your excess body hair", "Have you seen a dermatologist for your acne?" or "Have you tried this brand of cosmetics/supplements for your issues?". These prejudices can place a psychological burden on you, negatively affecting your self-confidence and mental health, and further exacerbating your PCOS symptoms.
PCOS can also impact your fertility and your relationship's future plans, creating a disconnect between you and others in your social circle who are at different life stages (e.g., starting a family). Whether you want children or not, the social pressure to meet traditional fertility norms can lead to feelings of shame and isolation, intensifying the stigma you may face. This situation can create a vicious cycle, affecting your self-confidence and worsening the psychological impacts of PCOS.
This social stigma can have devastating consequences. Several studies have highlighted an increased rate of self-harming behaviors or suicidal thoughts among women with PCOS compared to the general population (10). Additionally, women with PCOS have a suicide rate up to seven times higher than those without the condition.
In this first part, we've explored how PCOS can come with emotional challenges linked to the diagnosis and symptoms of the syndrome, leading to direct consequences on your mental health. Additionally, the hormonal disorders caused by PCOS can alter the functioning of your brain and stress response system, further impacting your mental health.
Despite these somewhat worrying findings about the potential effects of PCOS on mental health, in the second part of this article, we’ll explore how you can take steps to improve your mental health and feel better in both body and mind despite PCOS.🙂

PCOS: How to care for your mental wellbeing?
We have seen that PCOS can have significant impacts on your mental health, but that is not a life sentence! As with all your other symptoms, we’ll recommend best practices to help you achieve greater peace of mind.
The importance of medical follow-up for my PCOS
First and foremost, it's crucial to emphasize the importance of regular medical supervision for managing the general symptoms of PCOS. Whether it’s your GP, gynaecologist, midwife, or endocrinologist, these healthcare professionals play a vital role in ensuring that the progression of your condition is closely monitored. This helps to mitigate long-term risks associated with PCOS, such as the development of type 2 diabetes, heart issues, miscarriages, and pregnancy-related hypertension. They are equipped to provide a comprehensive diagnosis and, importantly, to rule out any other conditions that could explain the symptoms you’re experiencing that may not be linked to PCOS.
For a more detailed understanding of PCOS and its diagnosis, feel free to browse through our all our articles.
👉 Need clarity on your symptoms? Take our 2‑minute product quiz to see which supplements could help you.
You can also find recommendations for healthcare professionals specializing in PCOS on our Instagram page.
Additionally, seeking support from a mental health professional can be invaluable in helping you cope with both the physical and psychological symptoms of PCOS. Whether you choose to consult a psychiatrist, psychologist, or psychotherapist, it is essential not to isolate yourself and stay with deep-seated distress, as this can have serious consequences if left unaddressed (such as the development of psychological disorders or suicidal thoughts).
In cases of severe psychological distress, such as depression, anxiety attacks, or phobias, medical doctors and psychiatrists can prescribe medication to provide temporary relief while also guiding you to improve your mental health in the long term.
Alongside medical care, it's equally important for you to be as informed as possible about your condition and its implications for your overall health. Here's why:
The importance of education and awareness when it comes to PCOS
Understanding what’s happening to you is key, and this starts with educating yourself as much as possible about PCOS, its symptoms, and management. Raising awareness can encourage you to seek medical attention at the onset of symptoms, enabling early intervention, which is crucial to reduce the risk of long-term complications. Being educated about PCOS and its effects will also help you to better understand any medical treatment that may be prescribed to you, thereby enhancing their effectiveness. Additionally, this knowledge empowers you to take an active role in managing your symptoms on a daily basis, which can significantly improve your quality of life and mental well-being.
We also recommend that you involve one or more supportive members of your circle (a partner, parent, or friend) in your medical journey—what’s important is not to face this alone. Sharing your story with close friends and family, as well as more distant acquaintances (colleagues, etc.), helps to break the taboos surrounding this condition and fosters a better understanding of your experience. Raising awareness encourages a more empathetic approach, taking into account both the physical and mental aspects of your journey. Talking about your experiences can also educate healthcare professionals, promoting better overall management and holistic approaches for PCOS. Sometimes, your loved ones might not fully understand what you’re going through or might downplay the impact of PCOS on your daily life; this is why it’s vital to find support among people who truly understand you.
We recommend that you connect with online support communities. Facebook has several public or private support groups that can be very helpful. You can also join support and awareness associations such as Verity (the UK PCOS charity), which offers resources, events, and a supportive network. And, of course, you can always rely on the supportive SOVA community on our online platforms (Instagram/TikTok)! 🤗
Best practices to improve your mental health with PCOS
To start feeling better mentally, you might want to first focus on reducing the physical symptoms of PCOS by making some lifestyle changes. This includes your diet, which should ideally be anti-inflammatory and low glycaemic. To help you adjust your diet for PCOS, check out the article on our blog: The key rules of a diet adapted to your type of PCOS.
We also suggest reintroducing physical activities into your daily routine that are specifically tailored to PCOS. This can help improve your body image and self-esteem. These activities also have a positive impact on mental health (for more details, download our free e-book).
Incorporating wellness practices such as, for example, yoga, relaxation techniques, or coherent breathing into your daily routine can help reduce the impact of chronic stress on your body, and, in turn, alleviate the intensity of your symptoms. We’ll provide more insights into stress management techniques suitable for PCOS in an upcoming article. Of course, you can seek guidance from a healthcare practitioner such as a dietitian, nutritionist, specialist naturopath, sophrologist, or even a fitness coach to help you implement these changes.
To further boost your morale and mental health, we recommend a variety of activities:
-
Journaling: This practice involves keeping a “journal” (either a small notebook or a digital format) where you regularly note down your thoughts and emotions. You can also include uplifting collages, drawings, and decorations to enhance the therapeutic effect of writing. This can help you reduce anxiety, better manage your emotions, and halt the constant flow of negative thoughts.
-
Nature Walks: Being in nature—whether in a nearby park, forest, seaside, or greenway—can help clear your mind, shift your focus away from negative thoughts, and provide fresh air. Some studies have shown that spending time in nature positively impacts symptoms such as anxiety and even depression. (11)
-
Positive Affirmations: Based on the idea that the words you use can significantly impact your mindset and self-perception, integrating positive affirmations into your daily routine can boost your confidence, cultivate an optimistic outlook, and enhance your emotional well-being. Examples of affirmations include: “I am capable of overcoming challenges,” “I deserve success,” or “I am surrounded by love and positivity.” You can also find free recorded affirmations on platforms like YouTube, Spotify, or Deezer. Their positive impact on self-image has been well-documented. (12)
-
Photo Shoot: To reclaim your body and reconcile with your self-image, consider treating yourself (or having someone treat you) to a professional photo shoot where you’re the star you are for us! 😘Seeing yourself in a new light can help you develop a more peaceful relationship with your body and ease the negative emotions that might be tied to it (anger, sadness, frustration, etc.).
-
Digital Detox: We all know that nowadays, everyone is on social media. We spend a significant amount of time scrolling through images of “perfect” fake bodies, “dream lives,” and “tips to become the best version of ourselves.” This content can heighten negative thoughts about your image, personal experiences, and the challenges you face. Taking a “digital break” once or twice a year (for example, during your holidays) allows you to distance yourself from social media and better appreciate your own daily life.
-
Practicing Gratitude: Each day, try to note three positive things that make you feel grateful. These don’t have to be extraordinary; they could simply be “your pet”, a “comforting drink”, or a “smile from someone you passed by”. Focusing on these positive aspects will shift your attention to everything you already have in life rather than what you wish for but haven’t yet achieved. This practice helps to reduce anxiety, negative thoughts, and stress.
-
Feel-Good Content: Everything you listen to and watch influences your emotions and thoughts. This is why we recommend getting more content that makes you feel good and evokes positive emotions—such as comedy or romantic films and series, uplifting books, podcasts, YouTube videos, or music. It’s best to avoid anxiety-inducing, depressing, and stressful content (like the news, violent films and series, murder podcasts, etc.). Moreover, we encourage you to unfollow accounts that trigger feelings of inferiority or distance yourself from people whose behaviour or words might be toxic for you.
Finally, you can also support your mental health with certain dietary supplements that might help alongside the various lifestyle changes you’re making.

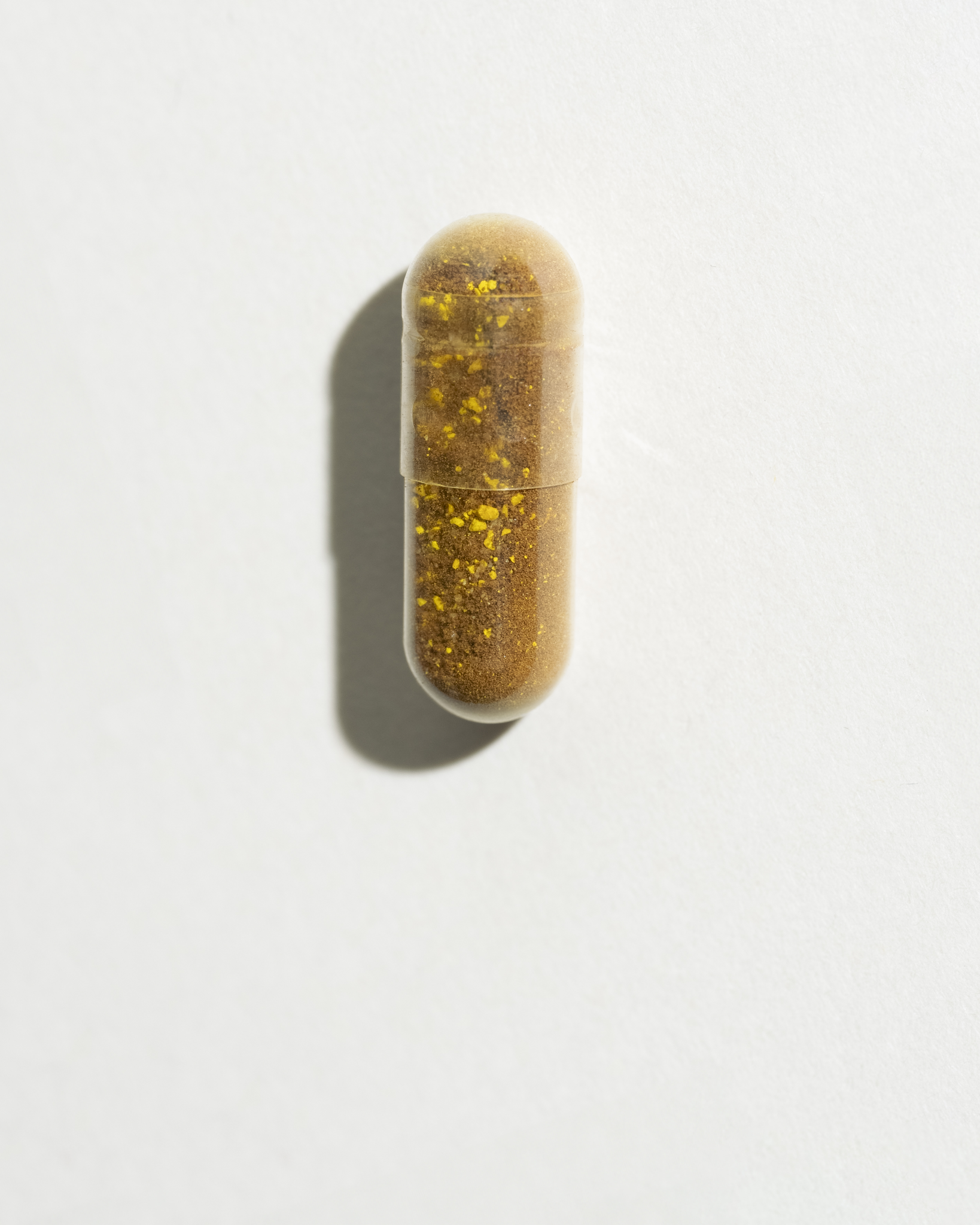
4 useful supplements to improve mental health
Supplements aren’t magic pills—but they can help balance hormones, reduce stress, and support your mood when combined with good habits.
✅ Ovastart – inositol + zinc to regulate cycles and reduce androgens
✅ Sugar Balance – helps manage blood sugar and reduce cravings
✅ Omega‑3s – for brain health and inflammation
✅ Magnesium & Vitamin D – calm the nervous system and boost mood
✨ For a simple start, try the Balance Bundle (Ovastart + Sugar Balance) — our best-seller for holistic PCOS support.
Adopting a holistic approach
In summary, this article has highlighted how PCOS can influence your mental health in several ways:
-
The condition presents significant emotional challenges (managing symptoms, potential infertility).
-
The physical symptoms of PCOS can disrupt stress and brain hormones, leading to increased anxiety and depression.
-
Social stigma surrounding the symptoms can also contribute to feelings of distress and isolation.
Despite these challenging aspects, there is hope for an improved quality of life through a holistic approach to managing PCOS. By integrating medical interventions, psychological support, lifestyle changes, and self-care strategies, it becomes possible to address both the physical and mental aspects of PCOS. A holistic approach not only tackles the physical symptoms of PCOS but also addresses the psychological repercussions of the condition. Your healthcare professionals, family, and society as a whole have a crucial role to play in supporting and understanding you.
Let’s remain hopeful! Growing awareness of PCOS is fostering a deeper understanding of the condition. Research continues, and we remain optimistic about the development of dedicated treatments for PCOS at some point in the future! Together, we can build a future where PCOS is not merely treated as a set of physical symptoms but where the mental and emotional needs of those affected are also recognised and addressed!
Scientific references
SOVA was created by two sisters with PCOS who wanted products that truly worked. Our formulas are developed in-house with women’s health and micronutrition experts, using ingredients backed by clinical studies and compliant with European regulations.
- Built by women with PCOS, we know the reality of the symptoms.
- Clinically studied, high-quality ingredients, including patented forms like Quatrefolic® and an optimal Myo-/D-Chiro Inositol ratio.
- Holistic support for hormonal balance, metabolic health, inflammation, mood and cycle regulation.
- Transparent, science-led formulas with no unnecessary additives.