Table of contents
What are the symptoms of PCOS - how can you obtain a diagnosis?
If you're reading this, it's most likely because you've recently been diagnosed with PCOS or have heard about the condition. Understandably, your mind is probably racing, and you probably have a million and one questions going around in your head.
PCOS: Behind these four letters hides a global hormonal dysfunction known as Polycystic Ovary Syndrome. It affects around 1 in 7 women (though experts believe this is likely an underestimate) and is the leading cause of infertility worldwide.
In this article, we’ll provide you with insights into the different causes and consequences of this condition, as well as details of how it can be managed.
🌸 PCOS : An overview
PCOS is a relatively common hormonal imbalance that affects women. It’s a condition that encompasses multiple factors: these include a disruption of hormones produced by the ovaries and the pituitary gland*, as well as changes in how the body functions.
This condition was discovered in 1935 by Stein-Leventhal, hence the name "Stein-Leventhal Syndrome", which it is also sometimes referred to as.
*The pituitary gland is a small gland located in the brain. Its main function is to produce hormones.
Symptoms of PCOS
Here are the most common symptoms experienced :
- Irregular menstrual cycles or no periods
- Acne
- Excessive hair growth in unusual places (chin, abdomen, etc.)
- Weight gain or difficulty losing weight
- Insulin resistance (which is also a contributing factor in PCOS)
- Chronic fatigue
- Hair loss
- Ovaries with a multifollicular appearance
- Difficulty conceiving
- Depression, stress, anxiety (our mental health article might help)
- Low sex drive
In terms of the symptoms mentioned by women afflicted with PCOS, this list is by no means exhaustive.
Diagnostic Criteria for PCOS
In the UK, the diagnosis of PCOS is based on a combination of medical history, blood tests, and imaging – usually an ultrasound scan of the ovaries (most often transvaginal for adults). Your GP will often refer you to a gynaecologist or sometimes an endocrinologist for further assessment.
Like most of Europe, the UK follows the Rotterdam criteria, recognised by the NHS and international health bodies.
According to these criteria, a diagnosis of PCOS can be made when two out of the following three signs are present:
-
Clinical or biological hyperandrogenism – this means either visible signs of high androgens (such as hirsutism, acne, or hair thinning) or raised androgen levels found on blood tests.
-
Irregular ovulation or anovulation – typically seen as irregular or absent menstrual cycles.
- Polycystic ovaries on ultrasound – showing a multifollicular appearance (20 or more follicles in at least one ovary, or ovarian volume above 10ml).
📝 Important: In the UK, an ultrasound is not recommended for teenagers unless they are more than 8 years past their first period, because multifollicular ovaries are very common during adolescence.
🖊 Examples of how a diagnosis might look in practice:
● Marie, 26 years old, suffers from acne (clinical hyperandrogenism) and hasn't had a period for 2 years (anovulation). However, her ovaries have a normal appearance during an ultrasound scan.
● Jade has irregular cycles (irregular ovulation) and on the ultrasound scan there are 20 visible follicles (ovaries with a polycystic appearance). She does not have acne or any other visible signs of hyperandrogenism.
● Zoé has not had an ultrasound scan, but she has 60-day cycles (irregular ovulation) and excessive hair growth (clinical hyperandrogenism).
💡 Did you know?
Other countries sometimes use different rules. For example, in the US, hyperandrogenism must be present for a PCOS diagnosis. But in the UK, any 2 of the 3 Rotterdam criteria are enough – as long as other conditions (like thyroid disorders or high prolactin levels) are ruled out first.

"Cysts" that are not really cysts
Vocabulary used to describe Polycystic Ovary Syndrome tends to revolve around the idea of "cysts," but we now know this is not the case.
When the condition was first discovered, doctors believed that the small masses visible on ovarian ultrasound scans were cysts. Today, we know they are actually follicles.
Follicles are small pockets where eggs mature. When an egg is ready to be released, the "dominant" follicle (the largest one) ruptures to let it pass: this is what is commonly known as ovulation.
For women afflicted with PCOS, eggs take much longer to mature than normal. This results in an accumulation of follicles in the ovaries. In simple terms: there is no dominant follicle; as a result, eggs remain in their small pockets and are not regularly released.
This creates what can best be described as a "traffic jam" scenario and gives the ovaries a "multifollicular" appearance on ultrasound scans. A more accurate term would be "ovaries with a multifollicular appearance."
*An egg cell is also known as a female gamete, as opposed to a sperm cell, which is the male gamete. If an egg cell is fertilised by a sperm cell, it becomes an "ovum." An egg cell is tiny, yet it is the largest cell in the human body !

The Different Types of PCOS
PCOS is often classified into four major categories. Please bear in mind that you may well fall into multiple categories.
It's not necessarily essential to fit into one of these boxes; the key is to actually identify the source of the imbalance for personalised management.
👉 If you want to discover the four types of PCOS, discover the 4 types of PCOS here!
Consequences of PCOS on women's health
PCOS is an ailment that can have multiple repercussions on a woman's health. It's important to know that this condition will unfortunately be present throughout your life; to date, there is no cure. However, by no means do we want to scare you; rather we want to make you aware that PCOS is a common ailment that requires comprehensive management.
So please don't worry : certain dietary habits, a healthy lifestyle, as well as targeted supplements can greatly improve the day-to-day lives of women afflicted by PCOS.
Infertility
It is often while trying to get pregnant that women discover they have the syndrome : absent or irregular ovulation significantly reduces their chances of conceiving.
Affected women are also at a higher risk of miscarriage simply because their egg quality is impacted by hormonal dysfunctions.
Read our article on how to get pregnant with PCOS for hope and guidance.
Insulin resistance
This is a complex phenomenon which will soon be addressed in its own dedicated article. In summary, hyperinsulinism and insulin resistance have numerous negative effects on the body :
● Hypersecretion of androgens
● Weight gain or difficulty losing weight
● Weakening of the immune system
● Digestive disorders
● Predisposition to type II diabetes
● Risk of cardiovascular diseases
Our Sugar Balance supplement is designed to support healthy insulin function.
Excess weight and Eating Disorders
Although not all women with PCOS are overweight, it remains one of the main risks of this condition. When excess weight is combined with insulin resistance, it becomes challenging to lose those excess kilos.
On the one hand, metabolic dysfunction hinders weight loss, and on the other, affected women often opt for sugar-laden foods.
Unfortunately, these difficulties can lead to many women modifying their eating habits, sometimes to extreme levels. It is not uncommon to see the exclusion of certain food groups, constant and intensive diets, and even anorexia or bulimia.
These behaviours need to be actively monitored as they can endanger a woman's health and plunge her into an anxious or depressive state. If you recognise yourself in any of these symptoms, please don't hesitate to seek the help of a competent healthcare professional whom you can trust.
Other Pathologies
Other pathologies may develop as a result of PCOS, such as hypothyroidism (which can also be a cause of PCOS) or cardiovascular diseases.
🎯 Tip: Many women find the Balance Bundle (Ovastart + Sugar Balance) helpful for tackling PCOS from multiple angles.
A Vague Diagnosis
The Rotterdam criteria are still debated in the scientific community. Some doctors believe that for a PCOS diagnosis, there should always be signs of hyperandrogenism — either:
-
Clinical hyperandrogenism: visible to the naked eye, such as acne or excessive hair growth.
-
Biological hyperandrogenism: detected only through blood tests.
In reality, some women are diagnosed with PCOS when their symptoms are actually caused by something else. This can delay proper treatment and make managing symptoms more difficult.
Many women with irregular or absent cycles also have ovaries that look “polycystic” on ultrasound. This makes sense — if there’s no period, ovulation doesn’t happen, leading to an accumulation of follicles in the ovaries.
But it’s important to know that irregular periods or no ovulation don’t always mean PCOS. Other conditions, like hypothyroidism, hypothalamic amenorrhea, or elevated prolactin levels, can cause similar symptoms.
👉 Don’t panic if you come across these complex terms — we’ll explain them in future articles!
What matters most is having trusted, knowledgeable healthcare professionals by your side. If you have doubts about your diagnosis, speak openly with your gynaecologist or doctor to make sure nothing is missed.
How to Manage Your PCOS ?
If you’ve made it this far, congratulations! By now, you’re probably wondering: “What can I actually do to get this under control?”
Your gynaecologist will likely bring up the contraceptive pill as a first option. The pill works by “pausing” your menstrual cycle — no cycle means fewer hormonal symptoms to deal with. It’s quick, it’s convenient, and for many women, it’s an easy solution.
But more and more women are looking for alternatives. Some don’t tolerate the pill well. Others simply want to explore more natural options — not to reject medicine, but to feel more in control of their bodies.
That’s where a natural approach comes in. This means looking at your diet, your lifestyle, and yes — the right supplements.
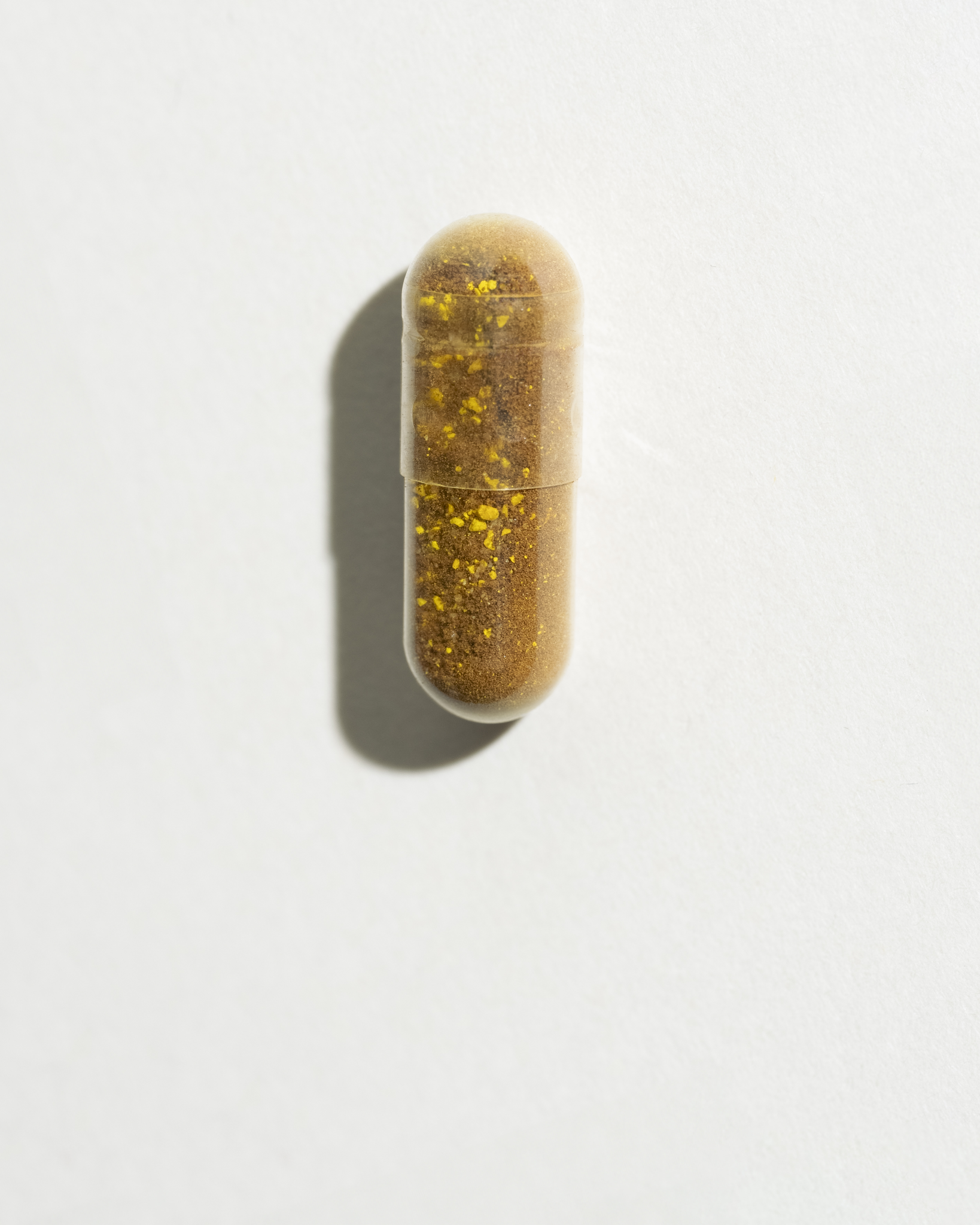
✨ Supplements like Ovastart (rich in inositol and zinc) can help regulate cycles, balance hormones, and support your overall reproductive health.
✨ If insulin resistance or sugar cravings are part of your PCOS picture, Sugar Balance combines cinnamon, berberine, and green tea to help manage blood sugar levels.
✨ And for those who want an “all-in-one” start, the Balance Bundle brings both together — a simple way to cover the foundations.
The truth is, there’s no one-size-fits-all solution. You might choose a medical approach (the pill), a natural approach (diet, lifestyle, supplements), or a mix of both.
Whatever you choose, one thing is non‑negotiable: a healthy diet and lifestyle are the foundation for managing PCOS and feeling better in the long run.
- Hormonal imbalance: PCOS involves disruptions in hormone production from the ovaries and the brain’s control gland, affecting ovulation and hormone levels. = Hormonal imbalance: PCOS involves disruptions in hormone production from the ovaries and the brain’s control gland, affecting ovulation and hormone levels.
- Hyperandrogenism: Elevated “male-type” hormone levels, which may lead to acne, unwanted hair growth (hirsutism), or thinning hair. = Hyperandrogenism: Elevated “male-type” hormone levels, which may lead to acne, unwanted hair growth (hirsutism), or thinning hair.
- Anovulation / Ovulatory dysfunction: When the ovaries don’t release eggs regularly; often leads to irregular or absent menstrual cycles. = Anovulation / Ovulatory dysfunction: When the ovaries don’t release eggs regularly; often leads to irregular or absent menstrual cycles.
- Multifollicular (polycystic) ovaries: Ovaries containing many small follicles (once thought to be “cysts”) visible on ultrasound; doesn’t always mean PCOS on its own. = Multifollicular (polycystic) ovaries: Ovaries containing many small follicles (once thought to be “cysts”) visible on ultrasound; doesn’t always mean PCOS on its own.
- Insulin resistance: The body's cells respond less effectively to insulin, which may contribute to weight gain, metabolic issues and exacerbate hormone imbalance in PCOS. = Insulin resistance: The body's cells respond less effectively to insulin, which may contribute to weight gain, metabolic issues and exacerbate hormone imbalance in PCOS.
SOVA was created by two sisters with PCOS who wanted products that truly worked. Our formulas are developed in-house with women’s health and micronutrition experts, using ingredients backed by clinical studies and compliant with European regulations.
- Built by women with PCOS, we know the reality of the symptoms.
- Clinically studied, high-quality ingredients, including patented forms like Quatrefolic® and an optimal Myo-/D-Chiro Inositol ratio.
- Holistic support for hormonal balance, metabolic health, inflammation, mood and cycle regulation.
- Transparent, science-led formulas with no unnecessary additives.