Table of contents
A quick refresher on PCOS
Polycystic Ovary Syndrome (PCOS) is a gynaecological and endocrine condition that remains somewhat enigmatic due to its multifactorial origins. It may have genetic and environmental causes or be triggered by hormonal upheavals—such as those experienced during pregnancy, after stopping the contraceptive pill, or following periods of significant stress.
At its core, PCOS often leads to an overproduction of androgens (male hormones such as testosterone). This hormonal imbalance disrupts ovarian function, resulting in anovulatory cycles—cycles where ovulation does not occur.
Since PCOS is fundamentally a hormonal condition, let’s explore the main hormones at play and how they become dysregulated.
What is a hormone?
Hormones are chemical messengers secreted by glands in the endocrine system—our body’s hormonal system. More than 50 hormones work together to maintain balance. Each hormone acts on specific “target cells” and can influence billions of cells at once, shaping everything from fertility to stress response.

Hormones in the menstrual cycle
It all begins in the brain, specifically the hypothalamus. This small region regulates the connection between the nervous system and hormone production.
The hypothalamus signals the pituitary gland to release FSH (Follicle-Stimulating Hormone) and LH (Luteinising Hormone), which then act on the ovaries. Together, these hormones regulate ovulation and the production of oestrogen and progesterone.
-
FSH stimulates the development of a follicle, the future egg.
-
LH surges mid-cycle (around day 14), triggering ovulation.
-
After ovulation, progesterone rises, preparing the body for a potential pregnancy.
If no fertilisation occurs, progesterone levels fall, triggering menstruation.
Menstrual cycle in PCOS
In PCOS, this delicate balance is disrupted. LH levels often remain chronically elevated, while FSH fails to surge. As a result, ovulation does not occur, leading to irregular or absent periods.
Key hormones of the cycle
-
Luteinising Hormone (LH): Usually peaks mid-cycle to trigger ovulation. In PCOS, LH remains abnormally high, contributing to anovulatory cycles.
-
Follicle-Stimulating Hormone (FSH): Stimulates follicle development. In PCOS, the surge never happens, so no dominant egg is released.
-
Oestrogens: Regulate the menstrual cycle, libido, bone density, and more.
-
Progesterone: Produced after ovulation by the corpus luteum. Low levels of progesterone are common in PCOS due to a lack of ovulation.

Other hormones involved in PCOS
Androgenic hormones
-
Testosterone: Naturally present in women at low levels. In PCOS, excess testosterone (hyperandrogenism) can cause acne, oily skin, hirsutism, or alopecia.
👉 If hair loss is one of your symptoms, our Scalp Serum is designed to support healthy hair growth. -
Delta 4-androstenedione: Produced by ovaries and adrenal glands. Elevated levels often indicate hyperandrogenism.
-
DHEA (Dehydroepiandrosterone): Mainly produced by adrenal glands, it’s a precursor to both oestrogens and testosterone. Elevated DHEA is common in PCOS.
Prolactin
Essential for lactation. High prolactin (hyperprolactinemia) is sometimes seen in PCOS and may contribute to amenorrhea (absence of periods).
SHBG (Sex Hormone Binding Globulin)
A liver-produced protein that binds testosterone and oestradiol, limiting their activity. Women with PCOS often have low SHBG, which increases free testosterone activity.
Other key hormones impacting PCOS
-
TSH (Thyroid-Stimulating Hormone): Regulates thyroid hormones. Imbalances can affect metabolism and menstrual cycles.
-
Cortisol: The stress hormone. Chronic stress can worsen PCOS symptoms by disrupting hormonal balance.
-
Insulin: Produced by the pancreas to regulate blood sugar. Insulin resistance—a key feature of PCOS—occurs when cells stop responding effectively to insulin. This is linked to weight gain, fatigue, and increased androgen levels.
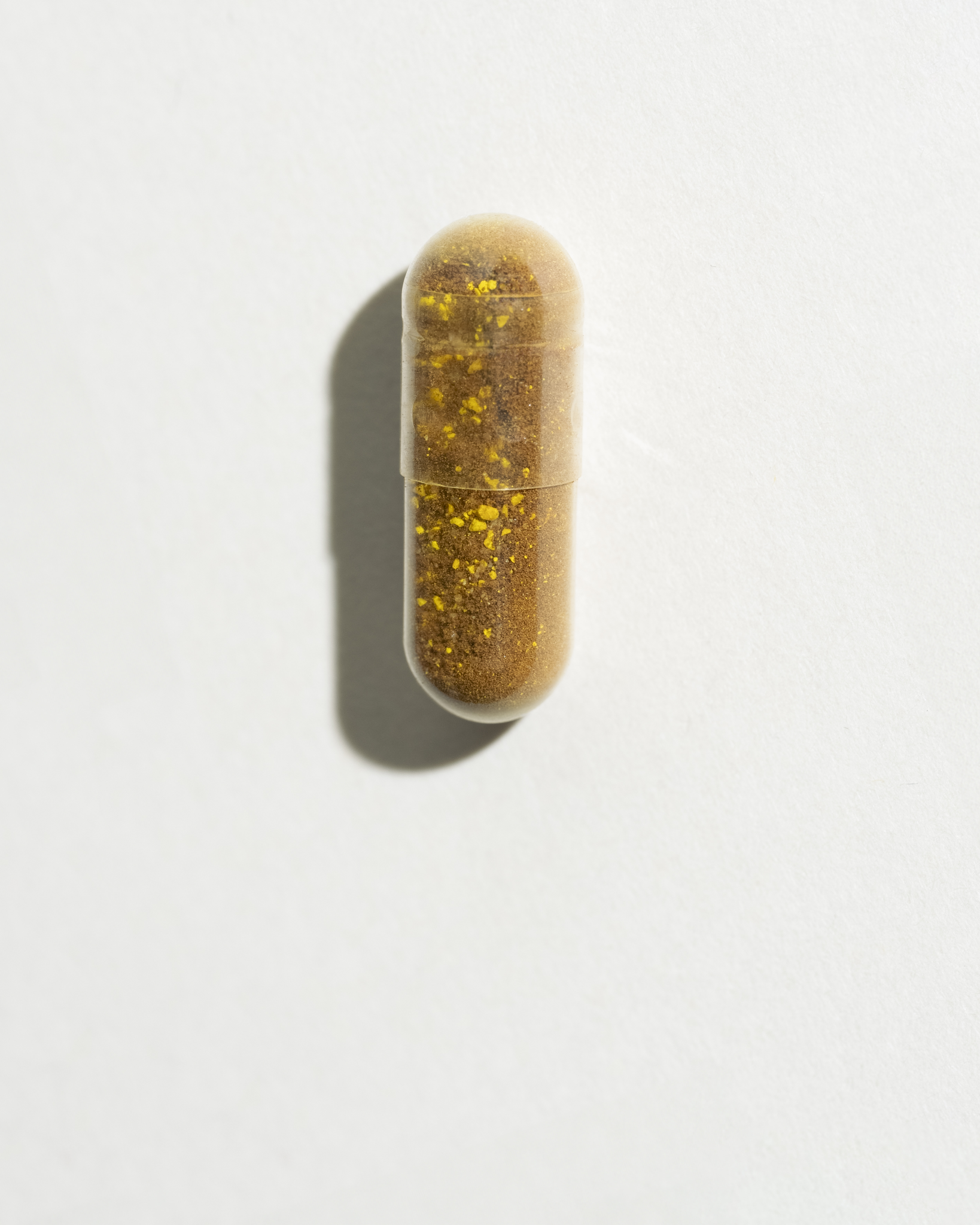
👉 Our Sugar Balance supplement is specifically formulated to support blood sugar balance in PCOS.
For a deeper dive, read our guide: How to lose weight with PCOS.
Understanding your own hormones
Each woman’s PCOS profile is different. Some struggle mainly with insulin resistance, others with androgens or thyroid involvement. That’s why getting personalised advice is essential.
👉 Not sure where to start? Take our Product Quiz to discover which supplements may best fit your symptoms.
Conclusion
Hormones are powerful messengers that regulate almost every function in our bodies. In PCOS, disruptions across several hormones—from insulin to testosterone—can create a cascade of symptoms.
Working with healthcare professionals, adjusting lifestyle factors, and supporting your body with the right solutions (from nutrition to supplements) can make a real difference in how you feel every day.
SOVA was created by two sisters with PCOS who wanted products that truly worked. Our formulas are developed in-house with women’s health and micronutrition experts, using ingredients backed by clinical studies and compliant with European regulations.
- Built by women with PCOS, we know the reality of the symptoms.
- Clinically studied, high-quality ingredients, including patented forms like Quatrefolic® and an optimal Myo-/D-Chiro Inositol ratio.
- Holistic support for hormonal balance, metabolic health, inflammation, mood and cycle regulation.
- Transparent, science-led formulas with no unnecessary additives.