Table of contents
Do you have PCOS and find yourself suffering from pain without really knowing what it's related to?
You might have talked about it with others, but it isn’t taken seriously, and you’re unsure how to ease it? Don’t worry, pain is a very common symptom of PCOS, though it’s often overlooked. Stay with us, and we’ll explain everything!
💡 If you want a complete overview of what is PCOS, its symptoms and management, you can start out with this article.
Pain: How does it work?
What is pain, and more importantly, what purpose does it serve? According to the International Association for the Study of Pain (1), which brings together doctors and researchers specialising in pain, it is described as an “unpleasant sensory AND emotional experience associated with actual or potential tissue damage.”
When faced with pain, a shock, or imminent burn, the body sends an electrical signal to the brain to warn it of danger. It functions somewhat like an alarm system to protect us.
Recent studies highlight the clear connection between the perception of pain and its emotional impact on the person who is injured. This is why pain is always a subjective experience, and everyone feels it with different intensities.
Today, the best way to evaluate pain perception is to ask the person to rate it from 1 to 10.
This is precisely what dozens of research teams have set out to understand—how the pain experienced by women with PCOS is perceived. We’ll explain it all in this article!

Health-related quality of life or HRQoL
When discussing polycystic ovary syndrome (PCOS), the conversation often focuses on hyperandrogenism, excessive hair growth, hair loss, difficulty losing weight, fertility issues, and so on. But do we talk enough about the pain that also forms part of the daily lives of women with this syndrome?
Numerous studies lament the lack of attention to this symptom, which nonetheless significantly diminishes the quality of life for more than one in seven women.
A 2022 study by a team of Chinese researchers shows that women with PCOS have an increased sensitivity to pain (2). The researchers synthesized over a hundred studies on the subject conducted in the past decade. All these studies relied on an HRQoL questionnaire (Health-related quality of life questionnaire). This questionnaire was filled out by hundreds of women with PCOS.
This questionnaire helps understand how a health disorder can alter quality of life in various life situations: relationships, sex life, family life, work, sports activities, and so on.
So, what are the conclusions of these studies? We’ll share them in the following paragraphs!
Women with PCOS have a greater sensitivity to pain
Several studies conducted in Germany and Poland show that the pain associated with PCOS—regardless of its location—significantly impacts quality of life. On the HRQoL questionnaire, the lower the score, the poorer the overall quality of life. The average score for women with PCOS is 36 out of 100. Surely, we can do better, right?
Not only do these studies show that pain impacts quality of life in general, but they also reveal that women with PCOS experience pain more intensely! This, in turn, further reduces their score.
But how is it possible that PCOS makes us feel pain even more intensely?
In this study, we observe that the symptoms of PCOS tend to lower the score. Whether due to physical discomfort (such as pelvic pain, physical discomfort related to weight, migraines, etc.) or psycho-emotional factors (discomfort due to excess hair, alopecia, acne, weight, etc.), it all plays a role. As mentioned earlier, emotions also affect the perception of pain!
In 2021, a study conducted in Spain showed that PCOS could reduce patients' optimism levels, thus increasing their pain perception. Interesting, isn't it?
Beyond this, physiological causes are also at play. The primary one is the process of chronic inflammation.
You can find more useful information on this subject in our article on Polycystic Ovary Syndrome (PCOS) Inflammatory: Explanations & Tips.

Chronic inflammation increases pain sensitivity in women with PCOS
The inflammation process is a natural action triggered by the body when it needs to defend itself. Whether it’s defending against an infection, pain, or other stimuli that may pose a danger to the body, this action triggers a rapid influx of immune cells (the body’s guardians) to the injured area (3).
When injured, this reaction is visible externally by swelling, redness, and/or warmth felt in the area. This is due to the blood flow, rich in immune cells, that causes these symptoms. Our body generally manages this inflammation well, as it’s a defense system.
There are two types of inflammation: acute and chronic. Acute inflammation is the one experienced temporarily during an injury or a short-term illness. It differs from chronic inflammation, which lasts over time.
Women with PCOS are often affected by what is known as low-grade inflammation, which is a milder inflammation with few symptoms. This type of chronic inflammation can further degrade the quality of life for women with PCOS by worsening their symptoms.
When inflammation occurs in the short term, it’s a sign that the immune system is functioning correctly, acting only when necessary. Chronic inflammation is a sign of a weakened or overactive immune system (as seen in autoimmune diseases) which, over time, can lead to:
- Chronic pain
- Hormonal imbalance
- Weight gain and/or difficulty losing weight
- Chronic fatigue
- Recurrent infections (e.g., cystitis, bronchitis, tendinitis)
- Musculoskeletal issues: osteoarthritis, fibromyalgia, etc.
- Signs of bacterial flora imbalance: vaginal yeast infections, intestinal disorders, etc.
- Mood disorders, depression, anxiety, etc.
Women with PCOS are more prone to chronic inflammation, which increases pain sensitivity. Therefore, it’s crucial to detect it early, manage it medically, and adapt one’s lifestyle accordingly.
What are the common pains associated with PCOS?
Generally speaking, the main pains women with PCOS face are as follows:
- Painful periods
- Pelvic congestion
- Weight-related pain (back, joints, etc.)
- Migraines
- Dyspareunia (pain during intercourse)
- Digestive pain
This non-exhaustive list varies according to each person's health profile!
Aggravating factors for PCOS-related pain
Low-Grade Inflammation
As mentioned earlier, chronic low-grade inflammation is a major source of chronic pain in women with PCOS. According to a study (2), PCOS-related hyperandrogenism is one of the factors that can exacerbate this inflammation.This contributes to the weakening of other metabolic processes which, in turn, will worsen the situation.
Insulin resistance
70% of women with PCOS suffer from insulin resistance. This refers to poor cell responsiveness to insulin, the hormone that is key to allowing glucose, or sugars, into the cells. This process promotes rapid weight gain with fat accumulation, particularly around the abdomen. Low-grade inflammation also fosters the development of insulin resistance.
This insulin resistance is also linked to the development of fibromyalgia in women with PCOS (4). A 2021 study showed that 100% of women with fibromyalgia in the volunteer group had issues with insulin resistance.
To learn more about insulin resistance, you can read our article Insulin Resistance and PCOS – What’s the Link?
Abnormal adiposity in women with PCOS linked to inflammation
Hyperandrogenism is one of the factors that trigger insulin resistance. The high level of androgen hormones and insulin resistance form an ideal combination for promoting abnormal adiposity. This refers to the accumulation of fat cells in the subcutaneous tissue. Adipocytes (the cells “specialised” in storing fat) accumulate, and through a series of biochemical reactions, they trigger a pro-inflammatory process (5). This inflammation, as a reminder, increases pain sensitivity.
Aggravating factors related to lifestyle
Lifestyle is crucial to preventing or managing chronic pain linked to low-grade inflammation. In a study using the Health-Related Quality of Life (HRQoL) questionnaire, researchers concluded that women with PCOS who do little or no physical exercise have a poorer quality of life and, generally speaking, more pain (6). This was particularly evident during the COVID-19 pandemic, which allowed studies on the impact of inactivity on the physical comfort of women with PCOS (7). A pro-inflammatory diet, stress, pollution, and endocrine disruptors will also promote chronic inflammation over time.
We’ll discuss the right habits to adopt shortly to help manage chronic inflammation-related pain better.
Pelvic congestion syndrome and PCOS
This syndrome is associated with varicose veins and/or venous insufficiency in the ovarian veins, leading to the dilation of blood vessels in the pelvic area. It can be the cause of chronic pelvic pain, particularly when standing for prolonged periods or during sexual intercourse. On average, this syndrome affects women aged 20 to 45, who have already had one or more pregnancies. The causes are still poorly understood and vary from woman to woman. Varicose veins in the ovarian area can lead to pain and localized chronic inflammation.
The congestion in the pelvic area linked to the multifollicular ovaries in PCOS can exacerbate this syndrome due to poor blood circulation, thereby increasing pain. These ovarian varicosities are detected through medical imaging and clinical examination.
If you experience chronic pelvic pain, do not hesitate to consult your gynaecologist to undergo the necessary tests and finally find relief!
Endometriosis and PCOS
A dual diagnosis of PCOS and endometriosis is possible. Many women report being affected by both conditions. Endometriosis is a condition characterized by the growth of tissue similar to the uterine lining outside the uterus. The most common symptom is severe pain, which worsens during menstruation and ovulation and can persist throughout the menstrual cycle. Pain during sexual intercourse and digestive issues can also indicate endometriosis. PCOS can also cause pain, as you’ve read here. If you recognise these symptoms, be sure to discuss them with your gynaecologist, who may recommend a pelvic MRI to diagnose endometriosis.
Now that we’ve understood the factors that can contribute to pain in PCOS, we won’t leave you without offering some solutions. We’ve put together a list of complementary techniques that are ideal for better managing pain associated with chronic inflammation.
A quick reminder: The origin of your pain must be diagnosed by a healthcare professional to avoid complications and similar issues. The tools we provide below can be used in addition to the advice given by your doctor and are not a substitute for medical follow-up.
Our best tips for managing PCOS-related pain
Manual techniques
Massage or plantar reflexology has proven effective in managing pain. These techniques allow you to reconnect with your body by experiencing positive physical sensations.
They promote better blood and lymphatic circulation, which helps reduce pelvic congestion syndrome, a common cause of daily discomfort, and painful periods and ovulations.
They also encourage muscle relaxation to ease pain that may be related to significant weight gain. A massage can relaxthe muscles, restoring comfort and mobility!
Their effect on emotional well-being is significant, as we now know that stress is a major factor in chronic inflammation. Emotions, as mentioned earlier, can either amplify or diminish the perception of pain.
This is a great reason to take care of yourself by enjoying a good massage or a reflexology session. 😉
Water in all its forms
These are all techniques that use the benefits of water for self-care. For managing pain associated with chronic inflammation, the sauna and steam room are ideal for promoting toxin elimination. The sauna, with its high, dry heat, helps eliminate toxins, reduces pain, strengthens the immune system, and improves blood circulation. The steam room is known for its stress-relieving effects, helping to ease muscle tension and also eliminate toxins.

In hydrotherapy centres, steam rooms and saunas are often located in places where you can also enjoy hydromassage jetsthat work more specifically on localised pain. Don’t hesitate to treat yourself to some time in these wellness-focused environments.
Another more common but equally effective method of hydrotherapy is the hot water bottle! Apply it to areas of pain and muscle tension to help you relax.
An anti-inflammatory diet
Whether as a preventive measure or during a flare-up, limiting foods that promote inflammation is important to reduce pain. This is especially true for inflammatory-related pain, which can vary greatly, including ovarian pain, digestive issues, migraines, joint pain, etc.
Here are our tips to avoid adding fuel to the fire:
- Avoid coffee and replace it with chicory, calming herbal teas, etc.
- Avoid refined sugar.
- Limit red meat consumption to two or three times a week.
- Avoid non-organic wheat (as its gluten is difficult to digest). Opt for ancient varieties of wheat (Kamut, Korosan, etc.) and organic farming. If these are hard to find, you can explore other alternatives as the general idea is to limit gluten.
- Avoid industrial products and favour homemade food as much as possible.
- Use anti-inflammatory spices like cinnamon, ginger, and turmeric paired with black pepper to season your dishes.
- A little bonus: remember to stay well hydrated throughout the day.
Want to learn more? Check our article dedicated to the key rules of a diet adapted to PCOS.
Engage in adapted physical activity
A lack of physical activity can contribute to musculoskeletal pain and increase the risk of diabetes, cardiovascular disease, and more. Engaging in daily physical activity is a significant advantage for living better each day. Choose an activity you enjoy, that makes you feel good, and that suits your physical condition. It will help prevent chronic joint and back pain, promote good venous return, and ensure proper blood circulation.
Dozens of studies have shown the benefits of yoga and stretching in preventing chronic pain(9).
Walking, hiking, cycling, and swimming are gentle activities accessible to most people. If your energy levels allow, don’t shy away from more dynamic sports like weightlifting, football, or karate. Have fun! We have an entire article to help you decide which sport you should be doing with PCOS, don't hesitate to check it out.
Why not consider joining a class near you, where you can be guided by an instructor who understands your pain and can tailor the activities accordingly?
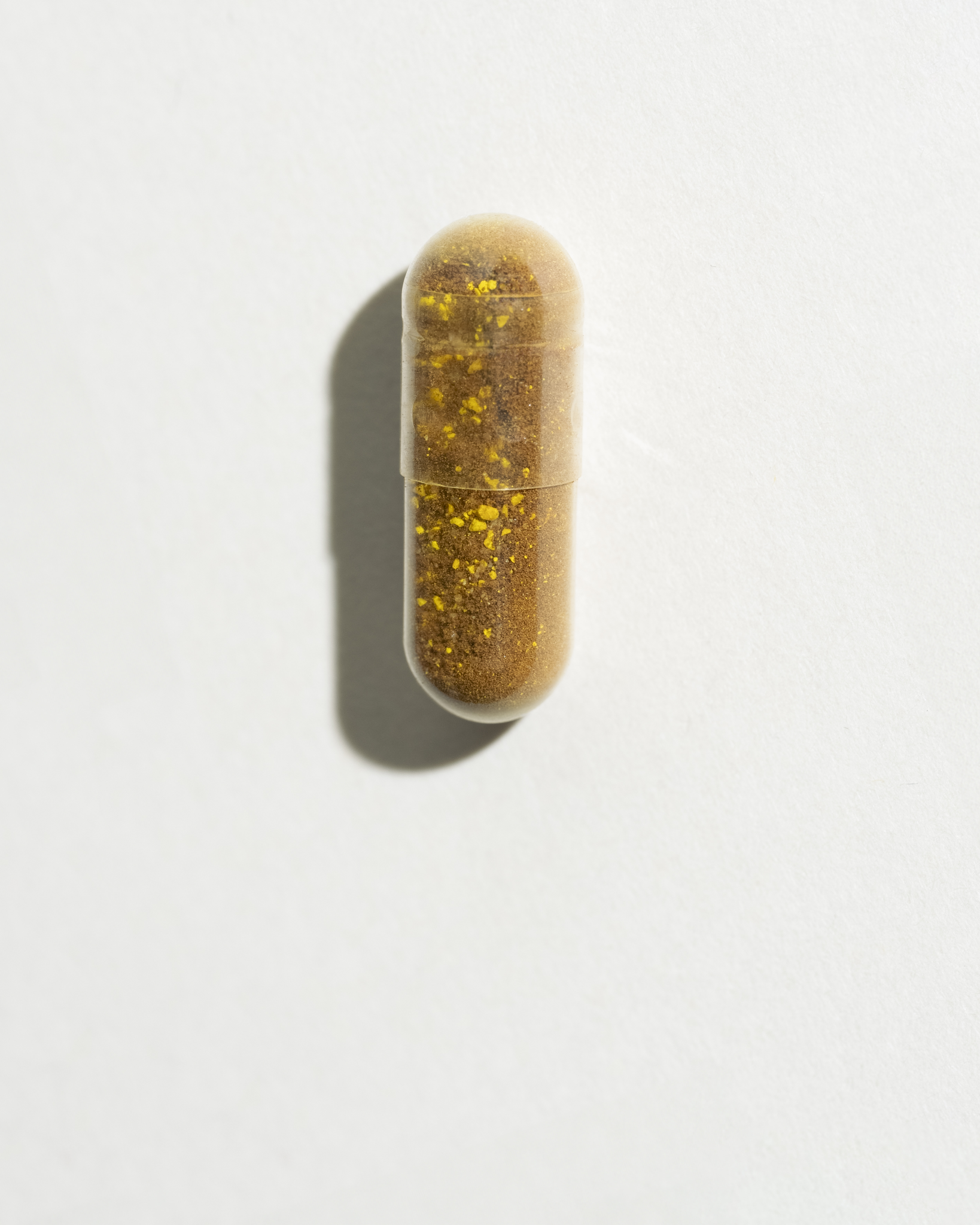
Micronutrition: aiding pain relief in PCOS
For painful periods
Over 70% of women with PCOS experience painful periods. Even if they only occur a few times a year, it’s helpful to know how to manage them better. Omega-3 fatty acides are ideal due to their anti-inflammatory properties at the uterine muscle level. They help to ease the contractions that cause pain. Paired with magnesium bisglycinate, which has muscle-relaxing properties, this will be an ideal combination to support you throughout your cycle
For dyspareunia
A study conducted in 2023 shows that sexual pain is common among women with PCOS (10). This pain can be related to muscle tension, stress, poor vaginal lubrication, pelvic congestion, an unsuitable IUD, etc. In such cases, the Omega-3 and magnesium duo is ideal (11). Don’t forget to supplement this with a visit to your gynaecologist or midwife to understand the cause of your pain.
For joint and back pain
As you’ve probably gathered, Omega-3 fatty acids (12) and magnesium are perfect for addressing inflammatory and musculoskeletal pain. This advice is applicable for these types of pain as well. It will also be important to understand the source of weight gain.
If it is linked to insulin resistance, as in 70% of women with PCOS, proper management is essential to prevent the development of type 2 diabetes.
For migraines
The source of migraines in PCOS is often hormonal. However, do not underestimate the emotional, physical, and environmental causes. Stress, poor sleep quality, inadequate hydration, and certain nutritional deficiencies are triggering factors.
If your stress is affecting your well-being, sleep, and causing headaches, our Serenity Booster is perfect for you! Its blend of adaptogenic and calming herbs helps to restore calm, and you can also combine it with magnesium bisglycinate to support the proper functioning of the nervous system.
For digestive pain
Finally, women with PCOS are often prone to intestinal issues, often linked to chronic inflammation. By affecting the health of intestinal cells, this inflammation impairs the proper absorption of nutrients. These nutrients, “poorly processed” by the epithelial cells, circulate in the bloodstream and promote further inflammation.
The best approach? Repair the intestinal lining with glutamine! This semi-essential amino acid is unmatched in calming intestinal inflammation and rebuilding the intestinal mucosal barrier. You need at least 3 grams of glutamine per day over three months to see long-term effects. Several labs offer this, so don’t hesitate to ask your naturopath for advice.
Of course, it’s essential to first check with a gastroenterologist to ensure there are no other concerns.
In these cases, also prioritise an anti-inflammatory diet, avoiding foods that you don’t tolerate well.
Take care of yourself
Most studies that contributed to the writing of this article highlight the lack of recognition of pain in the management of PCOS. Yet, it is very real and diminishes the quality of life for thousands of women. Don’t wait to take care of yourself—solutions exist, and we’re here to guide you!
💬 Not sure where to start? Take our PCOS product quiz to find out which supplement is right for you.
Scientific references
SOVA was created by two sisters with PCOS who wanted products that truly worked. Our formulas are developed in-house with women’s health and micronutrition experts, using ingredients backed by clinical studies and compliant with European regulations.
- Built by women with PCOS, we know the reality of the symptoms.
- Clinically studied, high-quality ingredients, including patented forms like Quatrefolic® and an optimal Myo-/D-Chiro Inositol ratio.
- Holistic support for hormonal balance, metabolic health, inflammation, mood and cycle regulation.
- Transparent, science-led formulas with no unnecessary additives.